Hunan University of Chinese Medicine researchers find acupuncture effective to treat functional dyspepsia (indigestion). Results from the investigation show that acupuncture is effective for easing upper abdominal pain and burning, nausea, and belching. In a semi-protocolized clinical trial, it proved two primary acupuncture points effective to treat functional dyspepsia (abdominal discomfort or pain with no known organic cause identifiable with endoscopy).
Electroacupuncture and manual acupuncture techniques were used to get treatment success. The total effective rates were 91.3% for upper abdominal pain, 90.62% for postprandial excess fullness, 95.45% for premature fullness, 93.33% for upper abdominal burning sensations, 87.5% for postprandial nausea, and 83.33% for belching. [1] This is significantly greater than scores in the sham acupuncture control group, which were never greater than 42.86% for any parameter.
Primary Acupuncture Points
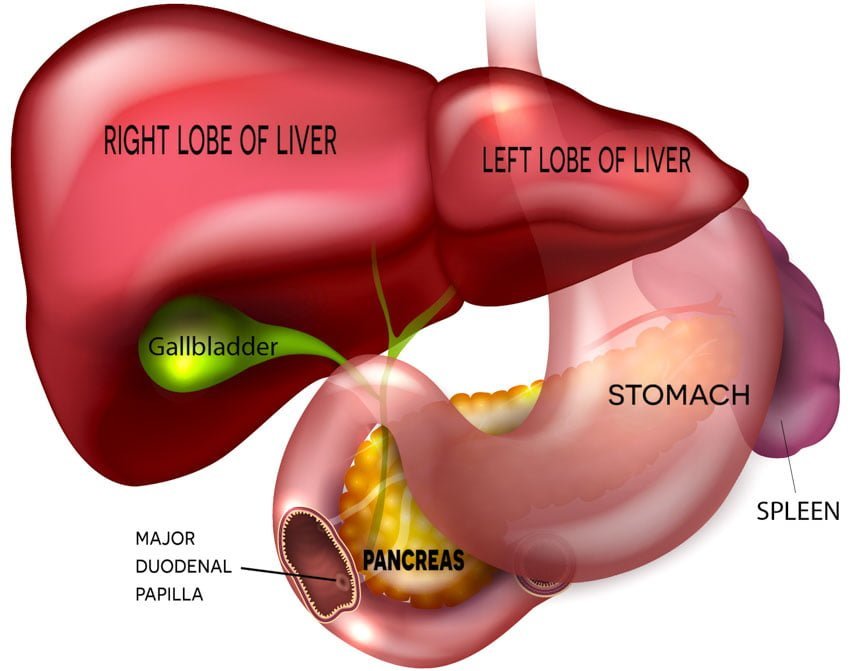
For patients in the acupuncture treatment group, they applied two acupoints to all patients: Zusanli (ST36), PC6 (Neiguan). The researchers commented on the point selection. They selected Zusanli for its location on the stomach foot yangming channel and its ability to treat all fu-organs (gallbladder, large intestine, small intestine, bladder, stomach, sanjiao). They add that Zusanli promotes the health of the spleen and stomach, dredges the channel, and regulates gastric tone and motility. [2] They note that Zusanli has been proven effective for patients with gastric motility disorders in prior research. Zusanli regulates gastric electrical rhythms relating to electrogastrographic power and gastric emptying time, secretion of gastrin and motilin, gastrointestinal hormones, and gastric acid (a combination of hydrochloric acid, potassium chloride, and sodium chloride). [3] The researchers also comment that Neiguan is indicated for relieving pain and promoting qi circulation and stomach health.
Additional points were added for specific diagnostic considerations. For patients with excess syndrome, Taichong (LV3) and Neiting (ST44) were added. For patients with deficiency syndrome, Gongsun (SP4) and Yinlingquan (SP9) were added. The researchers commented on the traditional use of these acupoints. Taichong is a yuan-source point on the liver channel and promotes health of the liver and stomach. Taichong promotes qi circulation and alleviates pain of the hypochondrium region. Taichong is also useful for treating emesis (vomiting) and abdominal bloating. Neiting is a ying-spring point on the stomach foot yangming channel. Both Taichong and Neiting are acupoints indicated for clearing heat from the liver and stomach channels.
Gongsun is located on the spleen foot-taiyin channel and promotes qi and blood circulation in the spleen and stomach channels. Gongsun regulates gastric acid secretion and prevents its excess. Yinlingquan is located on the spleen foot-taiyin channel and promotes qi circulation. Both Gongsun and Yinlingquan revitalize the stomach and spleen while activating qi circulation.
Acupuncture Procedure
Acupuncture points were applied unilaterally and sides were alternated every acupuncture session. Huatuo brand disposable acupuncture needles were used. All points were manually stimulated with a mild reinforcing and attenuating technique to achieve deqi.
Electroacupuncture was applied with a disperse-dense setting and the frequencies alternated between 2 Hz and 100 Hz at a 0.1–1.0 mA amplitude (based on patient tolerance levels) to all needles. Total needle retention time was 30 minutes per each acupuncture session. They applied acupuncture daily for five acupuncture treatments comprising one course of care followed by a two day break. They administered four courses of treatment to each patient.
To treat upper abdominal pain, the true acupuncture group outperformed the control group by 56.93%. For postprandial excess fullness, the acupuncture group outperformed the control group by 55.33%. For premature fullness, the acupuncture group outperformed the control group by 57.36%. For upper abdominal burning, the acupuncture group outperformed the control group by 64.76%. For postprandial nausea, the acupuncture group outperformed the sham acupuncture control group by 47.5%. For belching, the acupuncture group outperformed the control group by 40.47%.
Gongsun (SP4) and Neiguan (PC6)
In related research, investigators find acupuncture more effective than the drug mosapride to treat abdominal pain and discomfort because of indigestion. Specifically, acupuncture outperformed mosapride to treat functional dyspepsia. [4] The results were confirmed by electrogastrogram and other instruments. The acupoints used in the study were Gongsun (SP4) and PC6 (Neiguan), a classic eight extra channels confluent point combination.
The combination of Gongsun and Neiguan “significantly relieved clinical symptoms such as abdominal distention and discomfort after eating, early satiety, upper abdominal pain, and upper abdominal burning sensation.” The researchers note that “acupuncture outperformed drugs in regulating EGG dominant frequency and slow wave frequency.” They add, “compared with the drug group, the acupuncture group showed a significant difference in FDDQL scores.” [5]
They administered manual acupuncture and electroacupuncture. Patients rested in a supine position. Upon disinfection, a 0.30 mm × 40 mm acupuncture needle was inserted into each point, to a maximum depth of 25–40 mm. A mild tonifying and attenuating manual acupuncture manipulation technique was applied to achieve a deqi sensation. Next, they applied electroacupuncture with a disperse dense wave of 2–100 Hz (0.1–1.0 mA). They set intensity level to patient tolerance levels or until muscle contractions were observable. Electroacupuncture was applied once per day, 30 minutes per acupuncture session, for 30 days. For the control group, patients received 5 mg of mosapride citrate tablets, 30 minutes before meals. Tablets were orally administered three times per day, for 30 days.
They evaluated patients before and after treatment. First, they recorded improvements using a clinical scoring system. Next, a functional digestive disorders quality of life questionnaire (FDDQL) was recorded for each partient. Third, an electrogastrogram (EGG) was utilized to measure the electrical activity of the stomach (including EGG dominant frequency and slow wave frequency). The results indicate that acupuncture is both safe and effective to treat functional dyspepsia and acupuncture is more effective than mosapride. [6]
References
[1] Li DD, Yue ZH, Chao XL, Xie T, Hu GZ, Yang J. (2014). Evaluation of Long Term Effect of Electro Acupuncture on Patients with Functional Dyspepsia. Journal of Clinical Acupuncture and Moxibustion. 30 (2).
[2] Feng GX, Zhu Y, Jiang FD. (2004). The efficacy of conventional and auricular Acupuncture in treating Functional Dyspepsia (35 cases). Journal of Modern Chinese Medicine. 36(1): 48-49.
[3] Li YY. The effect of acupuncture on gastric acid secretion. (1991). Chinese Journal of Digestion. (6): 358.
[4] Hong Feng. Observations on the Efficacy of Electroacupuncture at Points Gongsun and Neiguan in Treating Functional Dyspepsia[J]. Shanghai Journal of Acupuncture and Moxibustion, 2016.
[5] Ibid.
[6] Ibid.